Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
Formulation and Evaluation of review on epilepsy and its management
Authors: Vikas Govind Kotkar , Prof. Latif Bagwan , Dr. L. D. Hingane
DOI Link: https://doi.org/10.22214/ijraset.2022.40688
Certificate: View Certificate
Abstract
In this project work we speak about different types of epilepsy. Epilepsy is 4th most common neurological disorder affecting 65 million peoples worldwide, according to epilepsy foundation of America, he found that approximately 45000 peoples are dead due to epilepsy. It is categorized into two main types i:e partial seizure( affecting small portion of brain) generalized seizures( covering all portion of brain). Several etiological factor responsible for causing epilepsy such genetic, CNS infection, metabolic disorders, miscellaneous. Epilepsy is caused due to imbalance between glutamate and GABA neurotransmitters. Abnormal jerking movement, confusion, fatigue, repetitive blinking are some common symptoms of epilepsy. While diagnostic test such as EEG, CT scan, PET scan, MRI and other treatment such ketogenic diet, vagus nerve stimulation, help to many people of all age who live with epilepsy. Today’s several antiepileptic drugs are available such as phenytoin, carbamazepine, ethosuximide, phenobarbital, may help to treat all types of epileptic seizures. So, there is need to continue research on it to treat all epileptic problems worldwide.
Introduction
I. INTRODUCTION
Epilepsy is a chronic disorder of the brain that affects people worldwide. Epilepsy is a chronic noncommunicable disorder of the brain hthat affects people of all ages.
It is characterized by recurrent seizures, which are brief episodes of involuntary movement that may involve a part of the body (partial) or the entire body (generalized), and are sometimes accompanied by loss of consciousness. There are over 2.5 million people diagnosed with epilepsy every year.
Epilepsy is one of 4th most common serious neurological disorder affecting about 65 million people globally. It affects 1% of the population by age 20 and 3% of the population by age 75. Nearly 80% of the people with epilepsy live in low and middle-income countries.
According to Epilepsy Foundation of America, he found that approximately 45,000 peoples are dead due to epilepsy. The estimated proportion is between 4 to 10 people /1000 is suffering from epilepsy.
During the 20th century, the invention of EEG, the advance in neurosurgery, the discovery of antiepileptic drugs, and the delineation of underlying pathophysiological mechanisms, were the most significant advances in the field of research in epilepsy . Now a days different antiepileptic drugs are available to treat seizure.
II. DEFINITION
A. Epilepsy is a disease due to central nervous system disorder which is characterized by seizures and convulsion or other abnormal body movements with loss of consciousness.
B. A seizure is defined by release of excessive and uncontrolled electrical activity in the brain. OR it is hyperexcitation of neurones in the brain leading to altered behaviour with or without violent motor activity.
C. Depending on the type of seizure, this can cause changes in sensation and feeling awareness and consciousness behaviour or movement
III. TYPES OF EPILEPSY/ SEIZURES
Classification of seizures are as either focal or generalized, based on how the abnormal brain activity begins.
A. Generalized Seizures
- Tonic-clonic seizures/ Convulsive seizures
- Absence seizures
- Tonic seizures
- Clonic seizures
- Atonic seizures
- Myoclonic seizures
B. Focal Seizures
Focal seizures (previously called partial seizures) start in one part of the brain and affect the part of the body controlled by that part of the brain or generally produced in a small area of the brain (fig no1). The symptoms the person experiences will depend on the function that the focal point is associated with or controls. Depending on where they start and which parts of the brain they involve, focal seizures may or may not alter consciousness or awareness , they can classified into two types.

- Simple Focal Seizures: These seizures do not result in loss of consciousness. They may alter emotion or change the way things look, smell, feel, taste or sound. They may also result in involuntary jerking of the body parts,such as an arms or legs, and spontaneous sensory symptoms such as tingling, dizziness, and flashing lights.
- Dyscognitive Focal Seizures: These seizure alter consciousness or awareness and may cause to lose awareness for a longer period of time. Dyscognitive focal seizures often result in starting and purposeless movements such as hand rubbing, chewing, swallowing, or walking in circles.
C. Generalized Seizures
Seizures that appear to involve all areas of the brain are called generalized seizures. Generalized epilepsy, also known as primary generalized epilepsy or idiopathic epilepsy, is a form of epilepsy characterized by generalised seizures with no apparent cause
- Bite your cheek or tongue
- Lick Your Jaw
- lose control of your bladder or bowels
- Turn Blue in the face
Many generalized seizures start and spread so quickly it is impossible to identify the source. If the source of a seizure is unidentifiable, surgery is not available as a treatment option.
Generalized seizures follow a basic pattern. First, your muscles stiffen and become rigid. Then, you experience violent muscle contractions in which the muscles move in quick, random spasms.
You lose consciousness, or black out, so that you’re no longer aware of what’s happening. The different types of generalized seizures are:
- Tonic-clonic Seizures: Tonic means stiffening, and clonic means rhythmical jerking Tonic–clonic seizures (formerly known as grand mal seizures) are a type of generalized seizure that affects the entire brain. A tonic-clonic seizure usually begins on both sides of the brain, but can start in one side and spread to the whole brain.
- Absence Seizures: Most commonly seen I children’s. Absence seizures are characterized by a brief loss of awareness, impairment of consciousness, blank stare, brief upward rotation of eyes. These type seizures last from few second to half of minutes.
- Tonic Seizures: These are the type of generalized seizures which causes stiffening of muscles. These seizure usually affects the muscles of arms and legs and may cause to fall to the ground. These types of seizures usually last 1 to 3 minutes and take longer for a person to recover.
- Clonic Seizures: Clonic seizures are associated with rhythmic, jerking muscles movements. These seizures usually affects the neck,face, and legs.
- Atonic Seizures: These are the type of generalized seizures which causes a loss of muscle control or tone, which may result in suddenly collapse or fall dow. Atonic seizures can be begin in one area or side of the brain (focal onset) or both sides of the brain (generalized onset). These seizures typically last less than 15 second
- Myoclonic Seizure: These are the type of generalized seizures usually appear as sudden brief jerks or twitches of arm and legs. During a myoclonic seizure, the person is usually awake and able to think clearly. Myoclonic twitches or jerks usually are caused by sudden muscle contractions, called positive myoclonus, or by muscle relaxation, called negative myoclonus.
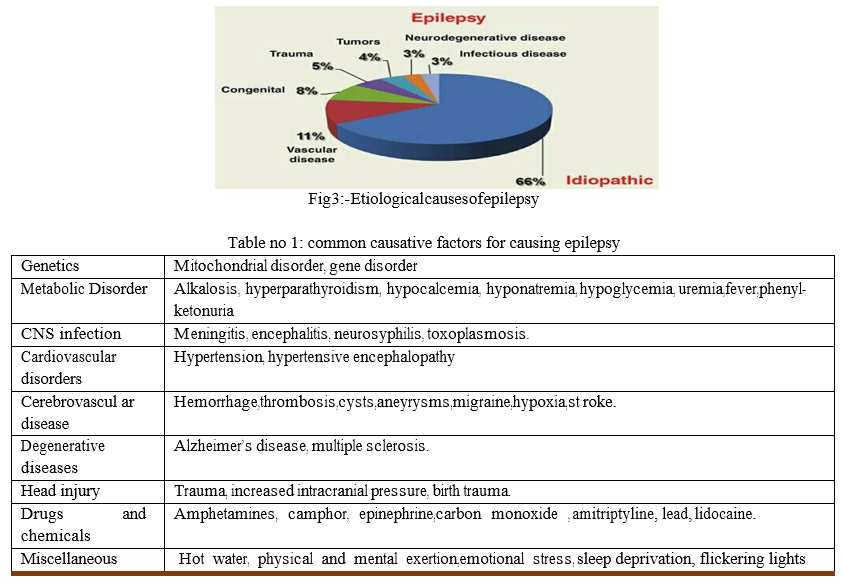
IV. ETIOLOGY / CAUSES
Many times the seizure are idiopathic in nature where exact cause6is not found. It may vary in peoples. Some people with no clear cause of epilepsy, but may have a some following causes which are responsible for epilepsy.
V. PATHOGENESIS OF EPILEPSY
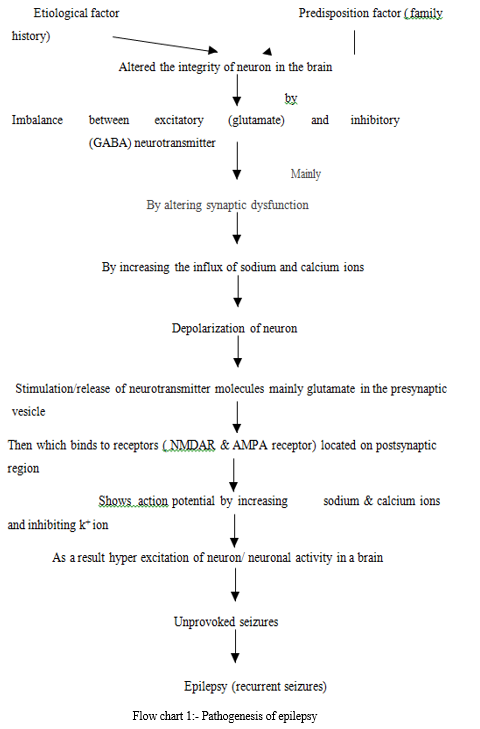
VI. PATHOGENESIS OF EPILEPSY
saCurrently, there is no universally accepted definition for epileptogenesis. The term epileptogenesis is defined as a process that leads to the occurrence of the first spontaneous seizure and recurring epileptiform events after the brain insult. OR Epileptogenesis is the process by which the previously normal brain is functionally altered and biased towards the generation of the abnormal electrical activity that subserves chronic seizures. Latency period refers to seizure-free or pre-epileptic periods between the brain insult and the occurrence of the first spontaneous seizure.
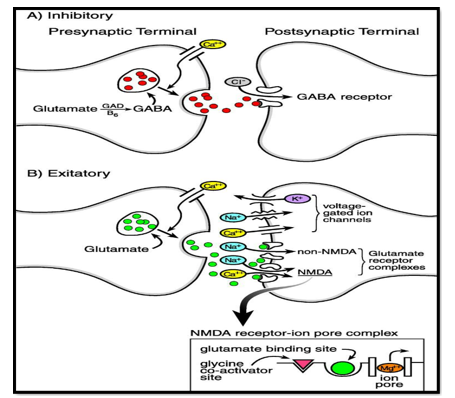
Fig 4:- Excitatory and inhibitory neurotransmitter involved in Pathogensis of epilepsy by binding to their specific receptor.
VII. SIGN AND SYMPTOMS
Following signs and symptoms are observed, if patients suffering from epilepsy.
- Loss of consciousness or awareness
- Uncontrollable/ involuntary jerking movements of arms and legs
- Visual hallucination
- Temporary confusion
- Alteration to sense of taste, smell, slight, hearing, and touch
- Performing repetitive movements
- Speech arrest, vocalizations
- Shaking
- Loss of bladder or bowel control
- Muscle stiffness, stiffening of body
- Episodes of staring
- Illusions
- Pupillary dilation/ eye rolling
- Repetitive movements of lip smacking and blinking
- Sometimes person goes in dreamy state
- Unusual fatigue
- Headache, nausea, vomiting
- Rapid heartbeats
- Sweating, excessive salivation
- Muscle spasms.
- Repetitive blinking of eyelids
- Altered mood
Table no 2:-Different epileptic seizures shows different sign and symptoms, they classified as following.
|
Sr.No |
Type |
Symptoms |
|
A |
Partial/ focal seizures |
Involuntary movement, unpleasant smell,taste,stiffening of limbs, altered emotion, nausea,seizure less than 2 min |
|
a |
Simple partial seizures |
Change in way of things,odd sound,smell,taste, dizziness, rising feeling in tummy,involuntary movements of body parts such as arms & legs, flashing lights. |
|
b |
Complex partial seizures |
Loss of consciousness, picking at cloths, smacking your lips, hand rubbing, chewing, swallowing, walking in circles |
|
B |
Generalized seizures |
Loss of consciousness or awareness, involuntary jerking movements of arms and legs, stiffening of body muscles, altered smell,taste,sound, seizures last less than 3 min. |
|
a |
Tonic-clonic seizures |
Stiffening or rhythmical jerking movements of arms and legs, shaking, increase heartbeats, loss of consciousness, biting tongue, difficult in breathing, loss of bladder control,lips may turn blue, seizures at least 1-3 min. |
|
b |
Absence seizures |
Blank stare, brief loss of consciousness or awareness, repetitive blinking, seizures at least |
|
|
|
few sec to half of min. |
|
c |
Tonic seizures |
Stiffening of muscles may cause to fall down, seizures at least 1-3 min. |
|
d |
Clonic seizures |
Mainly affect on neck, face or legs. |
|
e |
Atonic seizures |
Loss of muscle control or tone, results collapse or fall down, droop attack, seizures less than 15 sec. |
|
f |
Myoclonic seizures |
Sudden brief jerks or twitches of arms and legs, muscles contraction. |
VIII. DIAGNOSIS OF EPILEPSY
Epilepsy can be diagnosed by performing different test , they are given below. Your doctor may order several tests to diagnose epilepsy and determine the cause of seizures, they are given below
- Neurological examination
- Electroencephalogram (EEG) test
- Computerized axial tomography (CT scan CAT scan)
- Magnetic resonance imaging (MRI scan)
- Functional magnetic resonance imaging (fMRI scan)
- Positron emission tomography (PET scan)
- Complete blood count (CBC) test
- Chemistry panel
- Spinal tap test
- Single photo emission computerized tomography (SPECT scan)
- Magnetic resonance spectroscopy (MRS scan)
IX. COMPLICATIONS
Epileptic seizures create many complications, sometimes it is dangerous to human beings, they are given below.
A. Injuries and Accidents
- Injuries From Falls: Because many people with seizures fall, injuries are common. Although such injuries are usually minor, people with epilepsy have a higher incidence of fractures than those without the disorder. Patients who take the drug phenytoin have an even higher risk, since the drug can cause osteoporosis.
- Household Accidents: Household environments, such as the kitchen and bathroom can be dangerous places for children with epilepsy. Parents should take precautions to prevent burning accidents from stoves and other heat sources. Children with epilepsy should never be left alone when bathing.
- Driving and the Risk for Accidents: Being unable to drive is an extremely distressing and severe component of epilepsy. Drivers with well- controlled epilepsy are not at a high or unacceptable risk for automobile accidents. Uncontrolled epilepsy, however, poses a high risk. Needless to say, seizures can be very dangerous if they occur while a person is driving and result in injuries to the patient or others.
- Accidents while Swimming: Swimming poses another danger for people with epilepsy, particularly those with tonic seizures, which can cause the diaphragm to expel air quite suddenly. People with epilepsy who swim should avoid deep and cloudy water (a clear swimming pool is best), and always swim with a knowledgeable, competent, and experienced companion or have a lifeguard on site.
B. Status epilepticus:- (7)
Status epilepticus is a medical emergency in which seizures recur without the patient regaining consciousness between events. This condition can develop in any type of seizure but is most common in tonic-clonic seizures. Status epilepticus may cause brain damage or cognitive dysfunction and may be fatal. Subsequent seizures become briefer, more localized, and may be reduced to myoclonic activity.
C. Sudden Unexplained Death in Epilepsy (SUDEP)
Sudden unexplained death in epilepsy (SUDEP) occurs in a small percentage of persons with epilepsy. For reasons that are poorly understood, an otherwise healthy person with epilepsy can die suddenly. While this also happens within the general population, persons with symptomatic epilepsy have a much greater risk. Autopsies have not uncovered a physical cause of SUDEP. It is possible that pulmonary edema (fluid build-up in the lungs), suffocation, or cardiac arrhythmias (irregular heartbeat) may be responsible. Some people appear to be at a higher risk than others, such as young adults with generalized tonic-clonic seizures that are not fully controlled with medication and those who abuse alcohol and illicit drugs. Patients using two or more anticonvulsants may be at increased risk for SUDEP.
D. Effect of epilepsy on Children’s
- Long-term General Effects: In general, the long-term effects of seizures vary widely depending on the seizure's cause. The long-term outlook for children with idiopathic epilepsy (epilepsy of unknown causes) is very favorable. Children whose epilepsy is a result of a specific condition (for example, a head injury or neurologic disorder) have higher mortality rates than the normal population, but their lower survival rates are most often due to the underlying condition, not the epilepsy itself.
- Effect on Memory and Learning: The studies on the effects of seizures on memory and learning vary widely and depend on many factors. In general, the earlier a child has seizures and the more extensive the area of the brain affected, the poorer the outcome. Children with seizures that are not well-controlled are at higher risk for intellectual decline.
- Social and Behavioral Consequences: Learning and language problems, and emotional and behavioral disorders, can occur in some children. Whether these problems are caused by the seizure disorder and anti- seizure medications or are simply part of the seizure disorder remains unclear.
E. Effect of Epilepsy in Adults
- Psychological Health: Many adults with epilepsy show signs of depression. People with epilepsy have a high risk for suicide, particularly in the first 6 months following diagnosis. The risk for suicide is highest among people who have epilepsy and an accompanying psychiatric condition such as depression, anxiety disorder, schizophrenia, or chronic alcohol use. Antiepileptic drugs (such as carbamazepine, gabapentin, topiramate, valproate, and many others) can increase the risk of suicidal thoughts and behavior.
- Overall Health: Patients with epilepsy often describe their overall health as "fair" or "poor," compared to those who do not have epilepsy. People with epilepsy also report a higher frequency of pain, depression, anxiety, and sleep problems. In fact, their overall health state is comparable to people with other chronic diseases, including arthritis, heart problems, diabetes, and cancer. Treatments can cause considerable physical effects, such as osteoporosis and weight changes.
F. Effect On Sexual And Reproductive Health
- Effects on Sexual Function: Some patients with epilepsy experience sexual disturbances, including erectile dysfunction. Causes of these problems may be emotional, medication induced, or a result of changes in hormone levels.
- Effects on Reproductive Health: A woman’s hormonal fluctuation can affect the course of her seizures. Estrogen appears to increase seizure activity, and progesterone reduces it. Antiseizure medications may reduce the effectiveness of oral contraceptives. Epilepsy can pose risks both to a pregnant woman and her fetus. Some types of anti-epileptic drugs should not be taken during the first trimester as they can cause birth defects. Women with epilepsy who are thinking of becoming pregnant should talk to their doctors in advance to plan changes in their medication regimen. Women should learn about the risks associated with epilepsy and pregnancy, and precautions that can be taken to reduce them.
G. Effects of epilepsy on Pregnant Women
If the pregnant women suffering from tonic-clonic seizure, there is a temporary interruption of breathing; although this interruption rarely affects the mother, it can lead to oxygen deprivation in your baby. Additionally your baby’s heart rate can slow for as long as 30 minutes after a tonic-clonic seizure. This form of seizure also increases the risk of trauma to the baby. Tonic-clonic seizures present the greatest risk during the last trimester, when the baby’s brain is larger and needs more oxygen. Epilepsy can affect pregnancy in a variety of ways.
If seizures occur during pregnancy, a number of complications can occur affecting the baby including:
- Fetal heart rate deceleration
- Fetal injury
- Premature separation of the placenta from the uterus
- Miscarriage due to trauma experienced during seizures
- Preterm labor
- Premature birth
H. Anticonvulsant drugs
Epileptic women have a 4-6 % chance of having a baby born with a birth defect as a result of taking anticonvulsant drugs. Some are mild defects such as small fingers and toenails. However, there are more major birth defects such as spinal bifida, cleft lip, neural tube defects, and heart abnormalities. You should consult your doctor about your anticonvulsant medication when trying to become pregnant. They may recommend changing your medication or lowering the dosage of your current medication.
X. NON-PHARMACOLOGICAL TREATMENT
Different non pharmacological treatment available to control epileptic seizures or also treat them.
A. Ketogenic Diet
The ketogenic diet is a special high-fat, low-carbohydrate diet that helps to control seizures in some people with epilepsy. It is prescribed by a physician and carefully monitored by a dietitian. It is more strict, with calorie, fluid, and protein measurement and occasional restriction than the modified Atkins diet, which is also used today.
B. Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is designed to prevent seizures by sending regular, mild pulses of electrical energy to the brain via the vagus nerve. These pulses are supplied by a device something like a pacemaker.
C. Ayurvedic Treatment for Epilepsy:- (5)
In Ayurveda Epilepsy is known as Apasmara and the epileptic attacks are known as Akshpaka.
There are some herbs that are used in treatment of epilepsy. These are as following:
- Brahmi (Bacopa monnieri):-
a. It nourishes brain and helps in bringing coordination between nervous system and daily activity.
b. It acts as brain tonic.
c. It is also helpful in treatment of epilepsy, insomnia
d. It is helpful in all type of mood disorders. It is also helpful in relieving anxiety, stress and mental fatigue
2. Ashwagandha ( Withania somnifera)
It is best anxiolytic herb in Ayurveda.
a. It manages stress and anxiety.
b. It is nerve tonic, it has claiming effect on nerves.
c. It is very beneficial for the nervous system.
d. This herb possesses anti-inflammatory, anti-stress, immunomodulatory, antioxidant properties.
e. It is useful in increase mental and physical performance.
3. Jatamansi (Nardostachys jatamansi)
a. It is CNS relaxant.
b. It is best herb with tranquillizing effect on brain.
4. Tagar (Valeriana wallichii)
a. It helps to calming down nervous system.
b. It helps to relieve stress, depression and anxiety which are the underlying causes of epilepsy.
5. Shankhpushpi (Convolvulus pluricaulis)
a. It has mild anti-epileptic/ anticonvulsant property.
b. It help to reduce stress, depression, anxiety, dementia which are underlying causes of epilepsy.
D. Others
- Asan
- Yoga
XI. PHARMACOTHERAPY
Before going to Pharmacotherapy, the following guidelines for drug therapy must kept in mind.
A. Guidelines for Drugs Therapy:-(10)
- Before commencement of drug therapy, attempt must be made to uncertain the cause of seizure . Some seizures are successfully treated surgically. The choice of drug depends on the benefit-risk ratio of the antiepileptic. The objective of therapy is to control seizures as completely possible, without causing intolerable adverse reaction.
- Control should initially be attempted using a single drug therapy i:e monotherapy, choosen according to the type of epilepsy.The dose is increased until either the seizure cease or toxicity appear on combining antiepileptic drugs in most cases effect or additive.
- Anticonvulsant drug dosages must be individualized to avoid serious adverse reaction, or inadequate control whenever possible, plasma drug concentration must be monitored specially in patients on multiple drug therapy.
- All changes in drug therapy should be made as gradually as possible, with only one change at any one time, changes in dosages may be required from time to time.
XII. ANTIEPILEPTIC DRUGS
Antiepileptic (also commonly known as Anticonvulsant drugs or as Antiseizure drugs) are a diverse group of pharmacological agents used in the treatment of epileptic seizures. Anticonvulsants are also increasingly being used in the treatment of bipolar disorder and borderline personality disorder, since many seem to act as mood stabilizers, and for the treatment of neuropathic pain. Anticonvulsants suppress the excessive rapid firing of neurons during seizures. Anticonvulsants also prevent the spread of the seizure within the brain. antiepileptic drugs may block sodium channels or enhance γ-aminobutyric acid (GABA) function. antiepileptic drugs reduce the release of excitatory glutamate, whose release is considered to be elevated in epilepsy, they also act on voltage gated calcium channel.
A. Classification of antiepileptic drug:-(9,10)
- Anticonvulsant drug may be classified according to their chemical structure, they are given below.
- Barbiturate: Eg: phenobarbital, mephobarbital, pentobarbital
- Benzodiazepine: Eg: diazepam, clonazepam, nitrazepam
- Hydantoin:- Eg: phenytoin, ethotoin, mephenytoin.
- Succinimide:-Eg: ethosuximide, phensuximide, methsuximide.
- Oxazlidinedione:- Eg: trimethadione, paramethadione.
- Iminostilbine:- Eg: carbamazepine
- Valproic acid derivative:-Eg: Valproic acid, valproate sodium, divalproex sodium.
- Chemically unrelated anticonvulsant:-Eg: acetazolamide, primidone.
- Anticonvulsant drugs may be classified according to their mechanisms of action
- Enhancement of GABA action:- Eg: phenobarbital, benzodiazepine
- Inhibition of sodium channel:- Eg: carbamazepine, phenytoin, fosphenytoin, oxcarbazepine, lamotrigine
- Inhibition of calcium channel:- Eg: ethosuximide, valproate, trimethadione.
- Glutamate blockers:- Eg: felbamate, topiramate
- GABA receptor agonist:- Eg: phenobarbital clonazepam, primidone
- GABA transaminase inhibitors:- Eg: vigabatrin
- GABA analogue:- Eg: gabapectin, pregabalin
- Carbonic anhydrase inhibitors:- Eg: acetazolamide.
The main aim of antiepileptic drug is to inhibit abnormal neuronal discharge, the first three mechanisms are important.
Enhancement of GABA action: (19,12)
Gamma-Amino Butyric acid (GABA) is an amino acid which acts as a neurotransmitter in the central nervous system. It inhibits nerve transmission in the brain, calming nervous activity.
Phenobarbital: phenobarbital, also known as phenobarbitone or phenobarb, is a medication recommended by the World Health Organization for the treatment of certain types of epilepsy in developing countries. In the developed world it is commonly used to treat seizures in young children.
MoA: phenobarbital potentiate the effects GABA ( which is inhibitory neurotransmitters), by binding to GABA A receptor at different allosteric site as a result there is opening of chloride channel, due to which increased permeability of chloride ion/ increased influx of chloride ion into neuron which decreases excitability ( as a CNS depressant effect) by hyperpolarization of neuron.
Pharmacokinetic: Phenobarbital has an oral bioavailability of about 90%. Peak plasma concentrations are reached eight to 12 hours after oral administration. It is one of the longest-acting barbiturates , it remains in the body for a very long time (half-life of two to seven days) and has very low protein binding(20 to 45%). Phenobarbital is metabolized by the liver, mainly through hydroxylation and glucuronidation, and induces many isozymes of the cytochrome P450 system.
Dose: For children: 1 to 3 mg/kg
For adult 50 to 100 mg 2 to 3 times daily. Drug interactions:
a. Anticoagulants
- Phenobarbital lowers the plasma levels of dicumarol. Phenobarbital can induce hepatic microsomal enzymes resulting in increased metabolism and decreased anticoagulant response of oral anticoagulants (e.g., warfarin, , dicumarol)
b. Corticosteroids
- Phenobarbital appears to enhance the metabolism of exogenous corticosteroids probably through the induction of hepatic microsomal enzymes.
c. Griseofulvin
- Phenobarbital appears to interfere with the absorption of orally administered griseofulvin, thus decreasing its blood level.
d. Doxycycline
- Phenobarbital has been shown to shorten the half- life of doxycycline
E. Central nervous System Depressants
- The concomitant use of other central nervous system depressants including other sedatives or hypnotics, antihistamines, tranquilizers, or alcohol, may produce additive depressant effects.
F. Estradiol, estrone, progesterone and other steroidal hormones:
- Pretreatment with or concurrent administration of phenobarbital may decrease the effect of estradiol by increasing its metabolism.
Uses:
- Phenobarbital is used in the treatment of all types of seizures(except absence seizures) such as, temporal lobe epilepsy, clonic seizure, complex partial seizures, refractory seizures., tonic-clonic seizure, secondary generalized seizures, simple partial seizures, tonic seizures.
- Phenobarbital is the first-line choice for the treatment of neonatal seizures.
- Phenobarbital is sometimes used for alcohol detoxification and benzodiazepine detoxification for its sedative and anticonvulsant properties.
- Phenobarbital is a cytochrome P450 inducer, and is used to reduce the toxicity of some drugs
Side effects: Common side effects of phenobarbital includes, dizziness, drowsiness, confusion, depression, headache, nausea, vomiting, loss of appetite, weakness, aggression, problems with memory, constipation.
Benzodiazepine: Benzodiazepines (BZD, BZs), sometimes called "benzos", are a class of psychoactive drugs whose core chemical structure is the fusion of a benzene ring and a diazepam ring. Benzodiazepines enhance the effect of the neurotransmitter gamma-aminobutyric acid(GABA) at the GABAA receptor, resultingin sedative, hypnotic (sleep-inducing), anxiolytic(anti-anxiety), anticonvulsant, and muscle relaxant properties.
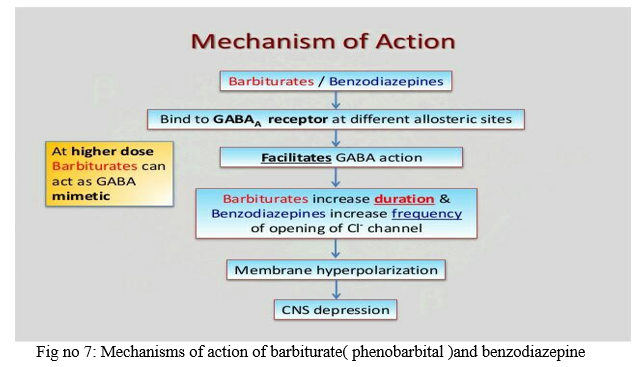
MOA Benzodiazepines work by increasing the efficiency of a natural brain chemical, GABA, to decrease the excitability of neurons. This reduces the communication between neurons and, therefore, has a calming effect on many of the functions of the brain.
Pharmacokinetic: Clonazepam is rapidly and completely absorbed after oral administration. The absolute bioavailability of Clonazepam is about 90%. Maximum plasma concentrations of Clonazepam are reached within 1 to 4 hours after oral administration. Clonazepam is approximately 85% bound to plasma proteins. Clonazepam is highly metabolized, with less than 2% unchanged Clonazepam being excreted in the urine. Biotransformation occurs mainly by reduction of the 7-nitro group to the 4-amino derivative. This derivative can be acetylated, hydroxylated and glucuronidated. Cytochrome P-450, including CYP3A, may play an important role in Clonazepam reduction and oxidation. The elimination half-life of Clonazepam is typically 30 to 40 hours.
Diazepam: diazepam are rapidly and completely absorbed after oral administration and it’s bioavailability is about 85%. These are also administered through IV and IM route , but onset of action is 1 to 5 min by IV and 15 to 30 min by IM route. These are metabolized in liver by glucuronidation. The biological half life is 15 to 20 hrs and shows long duration action about 10 to 20 hours. These are excreted through the kidney.
Uses: These are act as sedative and hypnotic for sleep disorders.
Benzodiazepine are used to control/ treat seizures eg clonazepam are used to treat myoclonic and absence seizure.
These are used to treat anxiety eg lorazepam. These are also act as muscle relaxant eg diazepam
These are used to treat insomnia and amnesia which are the underlying causes of epilepsy.
These are also used to treat panic disorder eg panic attack.
Side effects: drowsiness, dizziness, confusion, blurred vision (nystagmus) , agitation, headache, skin rash, hypotension, depression, impaired co-ordination, nausea, vomiting, inability to talk, coma, weakness.
Inhibition of sodium channel: (19,12)
Sodium currents are essential for the initiation and propagation of neuronal firing. Alterations of sodium currents can lead to abnormal neuronal activity, such as occurs in epilepsy. Within the central nervous system (CNS), VGSCs are critically important for regulating neuronal excitability, which are responsible for causing epilepsy. Influx of sodium ion through specific ion channels in the neuronal membrane causes a depolarization of neuron, which increases neuronal excitability.
Carbamazepine: Carbamazepine is a tricyclic compound chemically related to tricyclic antidepressants (TCA) with anticonvulsant and analgesic properties. Carbamazepine is used to prevent and control seizures. This medication is known as an anticonvulsant or anti-epileptic drug. It is also used to relieve certain types of nerve pain (such as trigeminal neuralgia). This medication works by reducing the spread of seizure activity in the brain and restoring the normal balance of nerve activity.
MOA: These drug act on voltage-dependent sodium channel and prevent the entry of sodium ions into neuronal membrane which are necessary for the generation of action potential. OR These drug bind preferentially to sodium channel and stabilize the sodium ions prolong in inactive state, inhibit the high frequency repetitive firing in neuron. These drug also decrease the synaptic transmission and increase the inhibitory effect of GABA.
Pharmacokinetic: Carbamazepine is relatively slowly but well absorbed after oral administration. Its plasma half-life is about 30 hours when it is given as single dose, but it is a strong inducer of hepatic enzymes and the plasma half-life shortens to about 15 hours when it is given repeatedly. CBZ is almost completely metabolized in the liver with only around 5% of the drug excreted unchanged. The major route of metabolism is conversion to CBZ 10.11-epoxide This reaction is primarily catalyzed by CYP3A4.
Uses: They are used to prevent and treat seizures
They are mostly used to treat generalized tonic-clonic seizure ( grand male epilepsy), partial seizure and psychomotor epilepsy.
They are used to treat nerve pain such as trigeminal neuralgia and diabetic neuropathy.
They are also used to treat bipolar disorder.
Side effects: Common side effects may include drowsiness, dizziness, headaches and migraines, motor coordination impairment, nausea, vomiting, and/or constipation.
Phenytoin: Phenytoin (diphenylhydantoin) is a hydantoin compound related to the barbiturates that are used for the treatment of seizures. It is an effective anticonvulsant for the chronic treatment of tonic-clonic (grand mal) or partial seizures and the acute treatment of generalized status epilepticus.
MOA: phenytoin binds to a voltage-dependent sodium channel and prevent the high frequency repetitive firing of action potential. This can be done by prolong inactivation state of sodium channel. Each sodium channel dynamically exists in the following 3 states:
- A resting state, during which the channel allows passage of sodium into the cell
- An active state, in which the channel allows increased influx of sodium into the cell
- An inactive state, in which the channel does not allow passage of sodium into the cell
Phenytoin that target the sodium channels prevent the return of these channels to the active state by stabilizing them in the inactive state so, they prevent repetitive firing of the neuron.
Uses: Highly effective in
-
- Tonic-clonic seizures
- Partial seizures ( simple, complex)
- Status epilepticus
- Arrhythmia
- Trigeminal neurologia
Common phenytoin side effects may include:
-
- dizziness, drowsiness, confusion, nervousness
- nausea, vomiting, constipation;
- tremors, slurred speech, loss of balance or coordination;
Ethosuximide:
Ethosuximide is an succinimide based anticonvulsant commonly used for absence (petit mal) seizures in both adults and children.
MOA: ethosuximide decreases low-threshold T-type Ca2+currents in thalamic neurons, and has no effect on the high voltage-activated Ca2+ currents. Ethosuximide reduces the peak amplitude of the low-threshold T-type Ca2+ current in the neurons of the thalamic ventrobasal complex, as well as in the reticular nucleus of the thalamus.
Pharmacokinetic:
- completely absorbed by oral administration
- Peak plasma concentrations is reached within 3 to 7 hours
- Negligible protein binding
- Completely metabolized in liver about 70 – 90%
- Half life 40 hours.
Uses: Ethosuximide is a first choice of drug for treating absence seizures. It is considered as second choice in myoclonic and atonic seizures.
Side effects:
-
- Central nervous system: drowsiness, mental confusion, headache, insomania ataxia.
- Gastrointestinal: nausea vomiting constipation cramps, dyspepsia, stomach pain loss of appetite weight loss swelling of tongue gum enlargement
- Blood: agranulocytosis, leukopenia, eosinophilia.
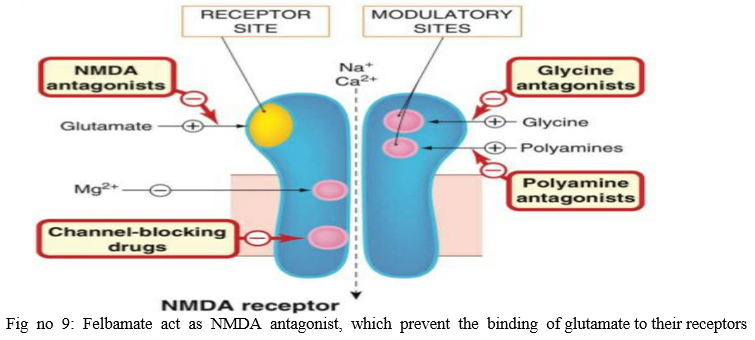
Glutamate blockers:(9)
Glutamate is a powerful excitatory neurotransmitter that is released by nerve cells in the brain. It is responsible for causing epilepsy ( excessive neuronal activity in the brain). So felbamate, topiramate , are the important drug to inhibit glutamate as neurotransmitters.
Felbamate:
These are the glutamate NMDA receptor blocker/ NMDA receptor antagonist which prevents binding of glutamate to N-methyl D aspartate receptor and inhibit abnormal neuronal activity.
Uses: effective against tonic-clonic seizure ( rarely)
Felbamate is also used to treat children with Lennox-Gastaut syndrome Side effects: aplastic anemia, hepatic failure, weight loss, GI irritation
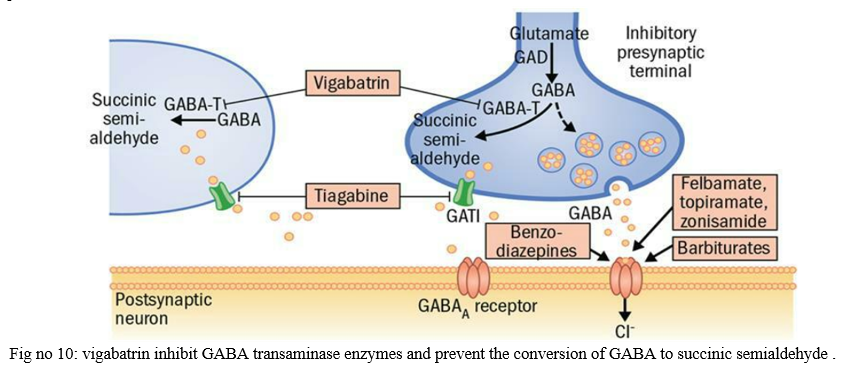
GABA transaminase inhibitor: (12)
GABA transaminase is an enzyme which catalyzes the breakdown of GABA to succinic semialdehyde So it is important to block the action GABA transaminase and enhance action of GABA.
Vigabatrin:
Vigabatrin is an antiepileptic drug that inhibits the breakdown of γ-aminobutyric acid (GABA) by acting as a suicide inhibitor of the enzyme GABA transaminase (GABA-T).
OR vigabatrin prevent the catabolism of GABA by irreversibly inhibiting the enzyme GABA transaminase, but does not bind to a receptor.
Use: It is used for treatment of adult refractory Complex partial seizure. Good first choice for infantile spasm from tuberous sclerosis.
Side effects
-
- Central nervous system: headache, dizziness, nervousness, memory disturbance, insomania, confusion.
- Gastrointestinal tract: headache nausea abdominal pain constipation dyspepsia.
Carbonic anhydrase inhibitors: Carbonic anhydrase inhibitors are a class of pharmaceuticals that suppress the activity of carbonic anhydrase. Clinically is used in treatment of glaucoma, epilepsy, neurological disorder and used as a diuretic.
Acetazolamide: acetazolamide inhibit carbonic anhydrase in the central nervous system to minimize the abnormal and excessive discharge from CNS neuron.
Common side effect include loss of appetite, vomiting, kidney stone, acidosis, liver problem.
Table no 4: Choice of proper antiepileptic drugs for specific type of seizures.
|
Type of seizure |
First line drug |
Second line drug |
|
Partial seizure |
Carbamazepine, phenytoin |
Gabapectin, Pregabalin |
|
Generalized tonic-clonic seizure |
Carbamazepine, Phenytoin, valproate |
Lamotrigine, clonazepam, oxcarbamazepine, |
|
Absence seizures |
Ethosuximide, valproate |
Acetazolamide, clobazam, |
|
Myoclonic / atonic seizures |
Valproate, sodium valproate, topiramate |
Clonazepam |
|
Tonic seizures |
Phenobarbital |
Gabapectin |
Conclusion
The treatment of epilepsy has been transformed since the serendipitous discovery of phenobarbital in 1912, both in the spectrum of medication available and improved knowledge of how best to use AEDs. Improving access to specialist information, as provided by the PwSI epilepsy service in primary care, encouraging adherence to medication combined with a rational combination of AED and concomitant medication, minimising side- effects and addressing any modifiable risk factors and addressing psychosocial issues can serve to optimise care for the patients with epilepsy.
References
[1] A book of neuropharmacology by Sloviter RS, Bumanglag AV, 2012. [2] A textbook of pathophysiology by Dr. S. L Bodhankar & Dr. N. S Vyawahare, Nirali prakashan, 10th edition 2016, Page no 3.5. [3] A textbook of principle of pathophysiology by Dr. C. M Jangme, R. D Wadulkar, Dr. M. D Burande, Dr. B. N Poul, Nirali prakashan, 1st edition 2015, page no 178 [4] A textbook of principle of pathophysiology by Dr. C. M Jangme, R. D Wadulkar, Dr. M M. D Burande, Dr. B. N Poul, Nirali prakashan, 1st edition 2015, page no 178 [5] Ayurvedic treatment of epilepsy authored by S Vidhya 2012 [6] Basic and clinical pharmacology by Bertram G Katzumg, Susab B Masters, Anthony J Trevor, tata McGraw hill publication, 12th edition 2010 page no 403. [7] Complication and prognosis of epilepsy authored by Frank Drislane and reviewed by Thaddeus Walczk, in 2004. [8] Epilepsy and its complication by Gordon R, Kelley MN, review in 2002. [9] Essential of medical pharmacology by KD Tripathi, JP brothers publishers, 7th edition 2013, page no 411.
Copyright
Copyright © 2022 Vikas Govind Kotkar , Prof. Latif Bagwan , Dr. L. D. Hingane . This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET40688
Publish Date : 2022-03-08
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

