Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
- Conclusion
- References
- Copyright
The Improvement of Balance, Coordination & Proprioception Following an MPI Cervico-Thoracic Junction Seated Adjustment: A Case Report
Authors: Dr. Brogan Williams, Dr. Michael Woodbury
DOI Link: https://doi.org/10.22214/ijraset.2022.46489
Certificate: View Certificate
Abstract
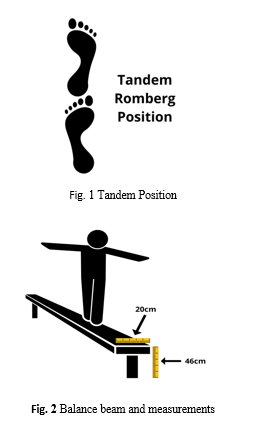
Further enquiries into how spinal manipulation directly impacts proprioception, balance and coordination are required to support the current body of evidence. The leading question of this study was “Does a Motion Palpation Institute cervico-thoracic junction high velocity, low amplitude adjustment impact proprioception, balance and coordination?”. A 32-year-old female with no prior gymnastic experience was recruited for this case-study. The participant was blind folded and given two attempts to maintain a static tandem Romberg stance on a 46cm high, 20cm wide gymnastic balancing beam for as long as possible. During the first attempt the participant lost her balance immediately. The participant then received a seated Motion Palpation Institute cervico-thoracic junction adjustment. Following the adjustment, an immediate improvement in balance, proprioception and coordination was observed. During attempt two, the participant could maintain her balance exponentially. The findings of this study suggest that spinal manipulation may have a potential benefit on proprioception, balance and coordination in a healthy patient. This further illustrates the importance of spinal manipulation as a non-invasive, low cost and low risk treatment. Further research to expand the findings of this study are needed to reach a stronger conclusion.
Introduction
I. INTRODUCTION
The knowledge and understanding pertaining to the mechanism of a chiropractic adjustment or spinal manipulation (SM) has been exponentially growing over the previous decade [1]. Many understand the benefits of SM regarding pain modulation and range of motion (ROM), however, there is less supporting evidence in the literature regarding proprioception, balance and coordination benefits (P.B.C) [2]. Further enquiries into how SM directly impact one’s P.B.C are required not only to support the current body of evidence but to provide more clarity on ways to develop the chiropractic standard of care. A stronger understanding and acceptance of such effects following SM is extremely important to further promote this treatment throughout the wider medical system. This is of extreme importance as it could provide aid to those suffering from kinesiophobia type illness/life threatening conditions where improvements in P.B.C could exponentially change their rehabilitation and movement outcomes. There have been some great studies conducted in New Zealand regarding the improvement of elbow position sense following cervical adjustments, and reduction in falls with elderly due to improvements in stepping reaction times and ankle joint position sense [3-4]. However, traditional methods were used to locate areas of the spine that required adjusting through an outdated “subluxation” based model, opposed to this case study, where the CTJ adjustment was given non-specifically without confirmation of traditional chiropractic “subluxation” findings – as this traditional belief of “subluxation” is not backed by science and widely not supported by mainstream medicine [5]. An MPI seated CTJ adjustment was chosen for its technical proficiency, comfort and the common subjective reputation of being a “wow” adjustment [6]. Established in 1981 by Dr. Len Faye and Dr. Maxwell Peterson, MPI has a strong reputation as being the top tier of chiropractors, not only because of their extremely competent technical skills but their progressive and bold shift of changing the chiropractic paradigm towards a more evidence-informed, integrated, functional model [7].
II. CONSENT
The participant was required to agree to a consent form prior to partaking in the case report. This was primarily to educate the participant on the study and to ensure they are 18 or above.
III. THE RESEARCH QUESTION
A. Research Question
Does an MPI cervico-thoracic junction HVLA adjustment impact proprioception, balance and coordination?
IV. METHOD
A 32-year-old female with no prior gymnastic experience was recruited for this case-study. The participant was blind folded and instructed to maintain a static tandem Romberg stance (heel to toe) on a 46cm high, 20cm wide gymnastic balancing beam for as long as possible. The participant had two attempts in total of which were timed by the researchers. Following the first attempt the participant received a seated MPI CTJ adjustment. The participant was then instructed to attempt the standing exercise again as the researchers observed whether there was any improvement in total standing time, indicating a possible improvement in balance, proprioception and coordination.
V. RESULTS
The participant failed immediately upon the first try having to place one leg down on the ground for stability. The participant then received a seated MPI CTJ adjustment. Both sides were adjusted with an audible cavitation present on each side. The participant noted immediate improvements in ROM. Following the adjustment, the participant was instructed to stand on the balance beam in the same fashion as the first attempt – the participant was blind folded and assumed a tandem static stance. An immediate improvement in balance, proprioception and coordination was observed. The participant could maintain her balance exponentially. The researchers stopped the timer at the 1 minute mark, but no deviations from her centre mass were observable. The increase in the participant’s ability to coordinate her body and maintain posture was remarkable and provided a rather conclusive result for this case study.
VI. DISCUSSION
The literature on SM over the past 20+ years has had wildly varying outcomes in regard to effectiveness in pain reduction, ROM improvements, and balance [8]. This is largely due to the lack of uniformity and consistency of what “spinal manipulation” entails. There’s a wide variety of different technical details in the application of SM between the three professions that most commonly utilize it globally (Chiropractors, Osteopaths, and Physiotherapists).
Even within the context of one of those professions (such as chiropractic) there is little uniformity between different schools of thought. There are pseudoscientific frameworks of understanding that influence various fractions of the profession on what SM does neurophysiologically and the differences in how to determine where and when SM needs to be applied, including variation in the deliverance of the “thrust” technique itself. We must also then consider how practitioners of different skill levels may influence the variation of care that is provided in terms of technique (since SM is in fact a skill that must be learned, practiced and improved upon over time). This amount of variation, that is almost never taken into account in studies on SM, has led to dramatic differences in what would qualify as proper SM technique, and may be a leading factor as to why some studies on SM show great improvements, and some are no better than placebo.
The choice to utilize MPI as the exclusive analysis and treatment protocol was due to their reputation of encouraging and teaching an evidenced-based understanding of SM and its neurophysiological effects, free from the pseudoscientific baggage the chiropractic profession has purported in the past. Its analysis is repeatable, thorough, and has a reputation of high inter-examiner reliability [9]. The technical aspects of SM through MPI are based on a functional model of chiropractic, which is supported by the current body of research [10]. MPI also understands that sometimes SM is contraindicated, not just for reasons of pathology but also in determining if areas of the spine would be considered hypermobile, thus not requiring SM. Perhaps the most important and clinically valuable paradigm of the MPI model is determining when not to perform SM, and understanding its limitations as an intervention [9].
P.B.C. is an important metric for determining mental status, potential intoxication levels, and ability for a person to be able to live independently and is widely observed and rehabilitated in a clinical setting for a variety of neurological, psychiatric, orthopaedic, or even dementia related illnesses [11]. Considering P.B.C. in healthcare decision making, as we globally face an aging and elderly population, is of great importance for doctors and patients worldwide.
The decision to use a participant with no prior gymnastics experience is a strength of this study, as it easily avoids a potential confounding factor of observing an individual who would possess a proprioceptive skill that could greatly skew the findings. Another strength of this study is the decision to blindfold the participant. Removing the utilization of the visual system from the study allows more specific testing of the brain structures in question, and correlates to standards of clinical examination of the cerebellum common in chiropractic practice [12].
The complete inability to maintain the tandem stance on the balance board prior to CTJ SM was noted, and not overly surprising given the lack of prior gymnastic experience. However, post SM, the researchers were surprised by the fact that the participant was not only able to maintain tandem stance, but that she continued to hold the position for over 60 seconds without any deviation from her centre of mass. This outcome strongly confirms the alternative hypothesis given earlier. After 60 seconds without any sign of loss of P.B.C. the researchers instructed the participant to dismount. The participant also reported increased ROM in the cervical spine post manipulation.
One potential limitation of this case study is the age of the participant. While the participant had no prior gymnastics experience, she was young and healthy, which could’ve played a role in her improvement post SM. Given her pre-existing state of good health, the effects of SM could have been amplified. Secondly, another confounding factor would be that she had better balance on the second attempt of the tandem stance merely by the fact that she had already tried once and had improved in skill from the prior attempt. This could lead one to believe that the participant would have had a better second try regardless of SM. However, the massive change in ability between attempts leads us to hypothesise that SM did have some contribution. A large limitation or confounding factor in SM is the skill level of the clinician delivering the manipulation. Like driving a car, shooting a basketball, or performing an Olympic lift, there is a vast difference in technical proficiency between beginners and experienced practitioners. This limiting factor is hardly unique to this study, however, the bilateral cavitation at the appropriate levels, and the increased ROM post SM confirms that this clinician was of good skill set, and an accurate representation of what a MPI based chiropractor would be performing in a clinical setting. Lastly, these results are of only one participant, not of a large sample size. There was no control group, so while the results from this case study are impressive and interesting, the real test would be repeating this procedure with a larger sample size; ideally with participants of various ages, sizes, and athletic backgrounds with some sort of control group, cross over clinical trial format and sham adjustment to account for potential placebo.
Conclusion
SM is commonly practiced by several prominent healthcare professions. Millions of people every year seek out SM to help with musculoskeletal ailments ranging from low back pain to headaches, with usually good outcomes. Given that musculoskeletal pain costs the global economy billions every year in missed work time [13], it’s evident that the safe and cost effective nature of SM is going to propel its utilization to levels never seen before. This makes research into all the potential benefits of SM critical in having a broader understanding of its uses, limitations, and appropriateness in treating many different problems patients could face. The findings of this study suggest that there is a potential benefit in proprioception, balance and coordination (P.B.C) from SM in a healthy patient. This further illustrates that the usage of SM in treatment for disorders that have a negative effect on P.B.C. could produce positive clinical outcomes, at very low cost and risk to patients. Although an insightful study, further research to expand the findings of this study is needed to reach a stronger conclusion.
References
[1] Haavik, H., Kumari, N., Holt, K., Niazi, I. K., Amjad, I., Pujari, A. N., Türker, K. S., & Murphy, B. (2021). The contemporary model of vertebral column joint dysfunction and impact of high-velocity, low-amplitude controlled vertebral thrusts on neuromuscular function. European Journal of Applied Physiology. https://doi.org/10.1007/s00421-021-04727-z [2] Williams, Dr. B. (2022). An Investigation into the Impact Spinal Manipulation May Have on the Performance of Strength Athletes: A Research Survey. International Journal for Research in Applied Science and Engineering Technology, 10(7), 1284–1291. https://doi.org/10.22214/ijraset.2022.45442 [3] Yang, J., Lee, B., & Kim, C. (2015). Changes in proprioception and pain in patients with neck pain after upper thoracic manipulation. Journal of Physical Therapy Science, 27(3), 795–798. https://doi.org/10.1589/jpts.27.795 [4] Holt, K. R., Haavik, H., Lee, A. C. L., Murphy, B., & Elley, C. R. (2016). Effectiveness of Chiropractic Care to Improve Sensorimotor Function Associated with Falls Risk in Older People: A Randomized Controlled Trial. Journal of Manipulative and Physiological Therapeutics, 39(4), 267–278. https://doi.org/10.1016/j.jmpt.2016.02.003 [5] Chiropractic Vertebral Subluxations: Science vs. Pseudoscience | Science-Based Medicine. (2010, October 1). Sciencebasedmedicine.org. https://sciencebasedmedicine.org/chiropractic-vertebral-subluxations-science-vs-pseudoscience/ [6] Cervical Thoracic Junction adjustment. (n.d.). Www.youtube.com. Retrieved August 4, 2022, from https://www.youtube.com/watch?v=DXyE7SNPDV4 [7] Motion Palpation Institute - About Page. (n.d.). Www.motionpalpation.org. Retrieved August 4, 2022, from https://www.motionpalpation.org/about [8] Ruddock, J. K., Sallis, H., Ness, A., & Perry, R. E. (2016). Spinal Manipulation Vs Sham Manipulation for Nonspecific Low Back Pain: A Systematic Review and Meta-analysis. Journal of Chiropractic Medicine, 15(3), 165–183. https://doi.org/10.1016/j.jcm.2016.04.014 [9] Schafer, R. C., & Faye, L. (1990). Motion palpation and chiropractic technique: principles of dynamic chiropractic. Motion Palpation Institute. [10] Ross, J. K., Bereznick, D. E., & McGill, S. M. (2004). Determining Cavitation Location During Lumbar and Thoracic Spinal Manipulation. Spine, 29(13), 1452–1457. https://doi.org/10.1097/01.brs.0000129024.95630.57 [11] Ide, R., Ota, M., Hada, Y., Watanabe, S., Takahashi, T., Tamura, M., Nemoto, K., & Arai, T. (2022). Dynamic balance deficit and the neural network in Alzheimer’s disease and mild cognitive impairment. Gait & Posture, 93, 252–258. https://doi.org/10.1016/j.gaitpost.2022.01.018 [12] Cohen, H. S. (2019). A review on screening tests for vestibular disorders. Journal of Neurophysiology, 122(1), 81–92. https://doi.org/10.1152/jn.00819.2018 [13] Bevan, S. (2015). Economic impact of musculoskeletal disorders (MSDs) on work in Europe. Best Practice & Research Clinical Rheumatology, 29(3), 356–373. https://doi.org/10.1016/j.berh.2015.08.002
Copyright
Copyright © 2022 Dr. Brogan Williams, Dr. Michael Woodbury. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET46489
Publish Date : 2022-08-27
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

