Ijraset Journal For Research in Applied Science and Engineering Technology
- Home / Ijraset
- On This Page
- Abstract
- Introduction
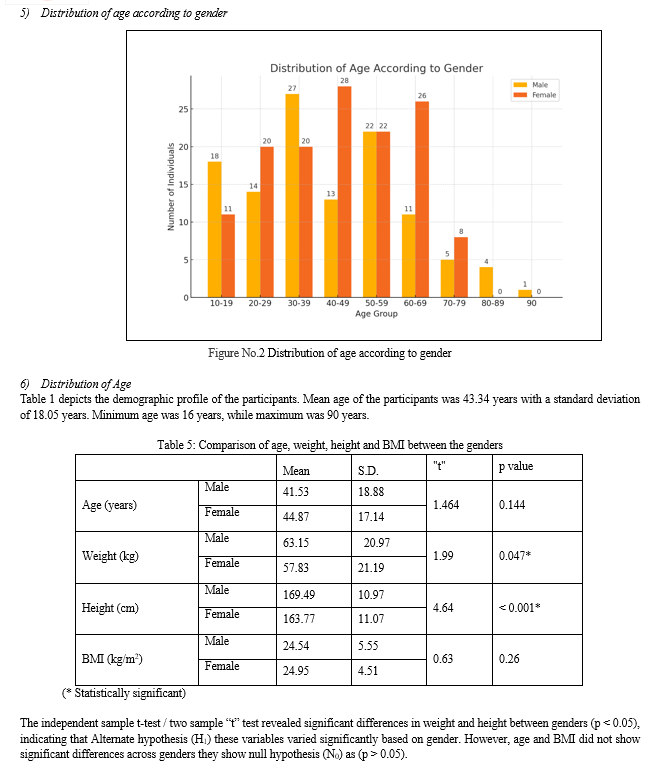
- Conclusion
- References
- Copyright
Studying the Optimal Air Volume Needed for Inflating the Cuff of an Endotrecheal Tube: A Clinical Observational Study
Authors: Urfeena Gani, Basiet Ali
DOI Link: https://doi.org/10.22214/ijraset.2024.63775
Certificate: View Certificate
Abstract
An endotracheal tube (ETT) is a polyvinyl chloride (PVC) flexible plastic tube, this tube is placed into the trachea through the mouth or nose. During the course of general anaesthesia or when a patient is unable to breath by him / herself the endotracheal tube is placed for the maintenance of breathing when it is necessary to sedate the patient, and airway protection is thus lost. Endotracheal tube is used for the protection of airway from any foreign body so that air can pass into and out of the lungs by which it can maintain the airway. This tube needs a special consideration with regards to cuff inflation for creating a seal in between trachea and endotracheal tube for preventing chances of aspiration and leakage of air. Therefore, we are conducting this study to find the optimal air volume needed to inflate the cuff of ETT and minimise the complications associated with over and underinflation of cuff. The conclusion of our study shows that There was a tendency to overinflate the ETT cuff, resulting in high intracuff pressure. The estimated optimal air volume needed for inflating the ETT cuff was about 6.05 ml for men and 5.45 ml for women.
Introduction
I. INTRODUCTION
Endotracheal tube is used for the protection of airway from any foreign body so that air can pass into and out of the lungs by which it can maintain the airway. Endotracheal intubation is primarily employed in situations such as surgical procedures conducted under general anaesthesia, wherein muscle relaxation, including the diaphragm, is necessary. It's also utilized to safeguard the airway from aspiration and to facilitate breathing during deep sedation or in cases of unconsciousness due to various causes. Endotracheal tubes are available in different sizes, and the most commonly used endotracheal tubes are 8.0 and 8.5-mm ID for males and 7.0 and 7.5 -mm ID for females. Endotracheal tubes are of different types: cuffed, uncuffed, Ring-Adair-Elwyn (RAE), flexo-metallic Endotracheal tube, Double lumen etc. The endotracheal cuff is inflated with air through a piolet balloon and because of its one-way valve the air will not leak back. To prevent the aspiration of gastric contents and secretions of upper airway. We should ensure the good positive pressure ventilation, for that the proper inflated cuff makes a seal with the tracheal wall. The cuff pressure should be maintained in between 20 to 25 H2O. Many complications may occur if it will exceed or subceed by the range.
Like other body hollow part, a delicate layer of tissue is lined in Trachea or windpipe called mucous membrane. This mucosal lining performs many useful functions to the body and while taking any intervention it needs to be taken care. When an endotracheal tube (ETT) is inserted and its cuff is inflated, it tightly presses against the tracheal lining, creating a reasonably airtight closure to block the escape of breathing gases and the entry of external secretions or foreign matter, a condition commonly referred to as aspiration. Therefore, excessive lateral pressure from the inflated endotracheal tube cuff can potentially lead to complete obstruction of blood flow to the underlying mucous membrane. Typically, the perfusion pressure (blood pressure responsible to drive the blood across capillaries, ending up in perfusing tissues) falls within the bracket of 30 to 40 mmHg.1 If any hemodynamic disturbance results in a decrease in systemic blood pressure, perfusion pressure will similarly decrease. Therefore, it’s essential to ensure the lateral pressure applied by the ETT cuff does not surpass the mucosa’s tolerance. Otherwise, insufficient blood supply could lead to ischemia, cell death in the mucosa, scarring, and ultimately damage to the trachea. In its mildest manifestation, patients might experience only minor discomfort such as a mild sore throat. However, in more severe instances, the pressure from ETT and cuff can result in lasting complications, including ulceration of the tracheal lining, tracheal stenosis, subglottic stenosis, tracheal rapture, formation of tracheal granulomas and recurrent laryngeal nerve injury. These complications can be serious enough to necessitate multiple surgical interventions. Finding the optimal inflation level is essential for patient’s safety and comfort, achieving a balance is crucial to avoid both under-inflation and over inflation of the cuff, too less inflation of cuff can permit gas leak and aspiration leading to the loss of blood supply to the mucous membrane.
Therefore, it is crucial to maintain ETT cuff pressure within the safe range of 20 to 30 cmH2O. However, the consultant anaesthesiologists and anaesthesia caregivers often inflate the cuff to an arbitrary volume or pressure based on clinical judgment for two main reasons. Firstly, a pressure gauge might not be immediately available. Secondly, during emergency procedures, time constraints may lead to overlooking the importance of regulating ETT cuff pressure. Consequently, we investigated the average inflation pressure of ETT cuffs after routine intubation and the amount of air used for inflation. We also estimated the difference between the volume of air used and the volume required to inflate the cuff to 25 cmH2O.
II. MATERIALS AND METHODS
- Ethics Consideration: We took the permission from hospital organization ethical committee before starting this study
- Study Approach: The study was conducted in the department of anaesthesiology Ahmed hospital Srinagar J&K India
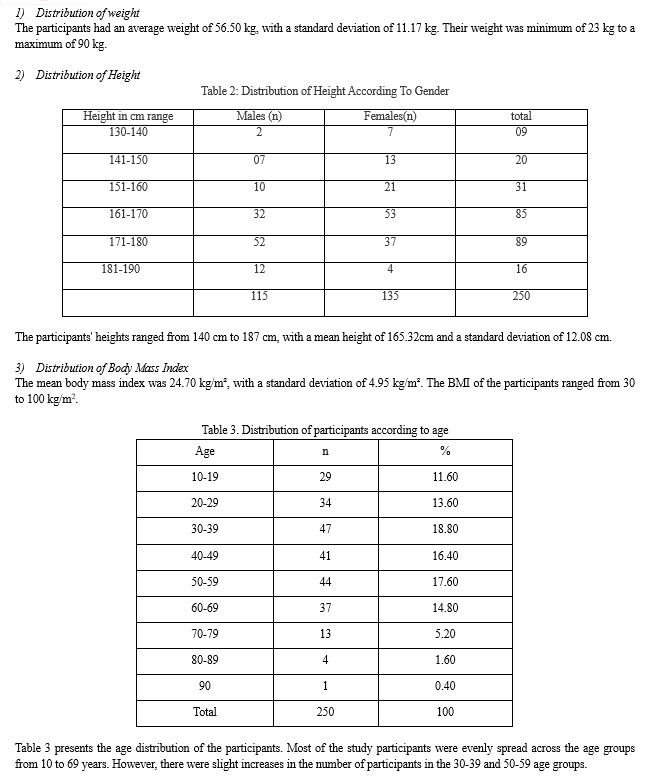
- Study Design: it was a clinical observational cross-sectional study Patients scheduled for elective surgery under different diagnosis in general, gynaecology & ENT surgery whose surgery was performed under general anaesthesia and require endotracheal intubation.
- Study Materials: Endotracheal tube (Romsons® Endotracheal tube Romson Group Private Ltd. Industrial Estate, Nunhai, Agra UP India & Portex®, Smiths Medical ASD Inc, Minneapolis, USA), Endotracheal tube cuff manometer (Pulmodyne cuffcheck Aneroid cuff pressure manometer, Indianapolis USA) and 10 ml & 20 ml syringe (Dispovan HMD India).
- Sample Size: 250 patients were included in the study to ascertain the quantity of air necessary to attain a cuff pressure of 25cm H2O.
A. Inclusion Criteria
- These Consecutive patients underwent elective surgery under general anesthesia requiring ET Tube intubation.
- General surgery
- Elective Gynecological procedures
- ENT Procedures
B. Exclusion Criteria
- Patients with facial trauma or other craniofacial abnormalities affecting airway management
- Patients with suspected difficult airway, Significant upper airway obstruction.
- Patients with known allergies to the materials used in the endotracheal tube or cuff
- Pregnant patients
- Patients with full stomach symptoms/ signs of GERD
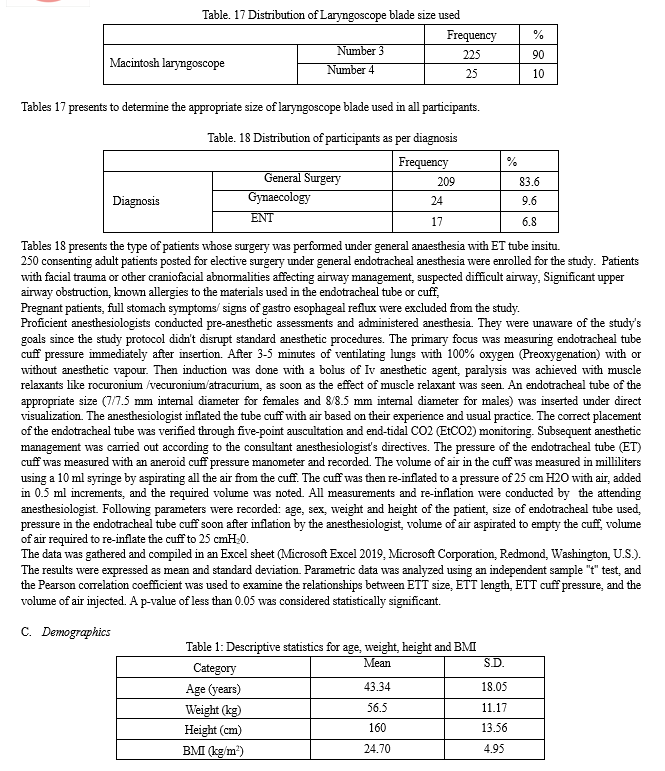
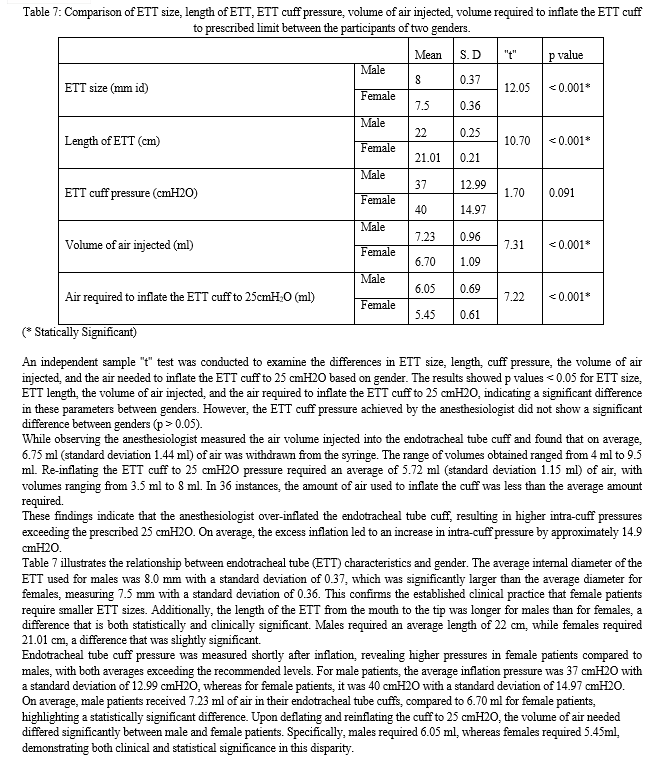
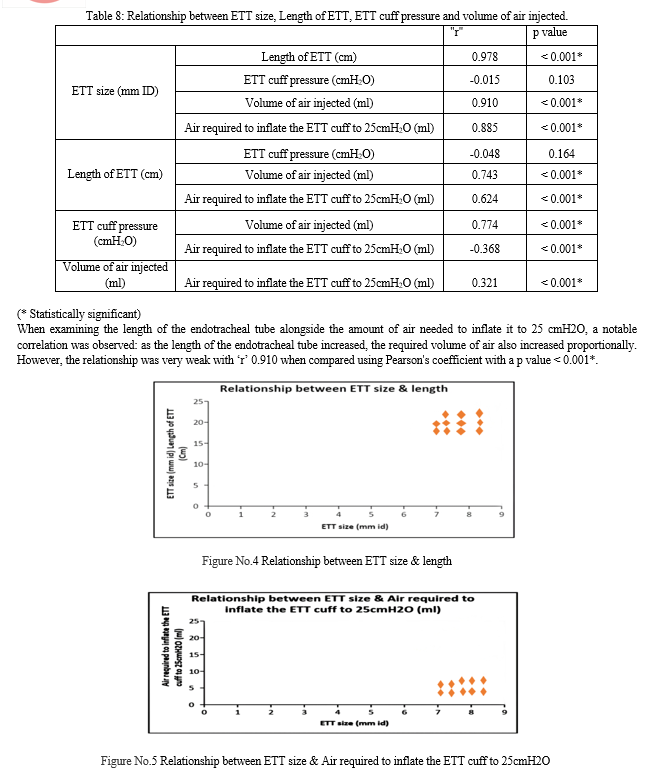
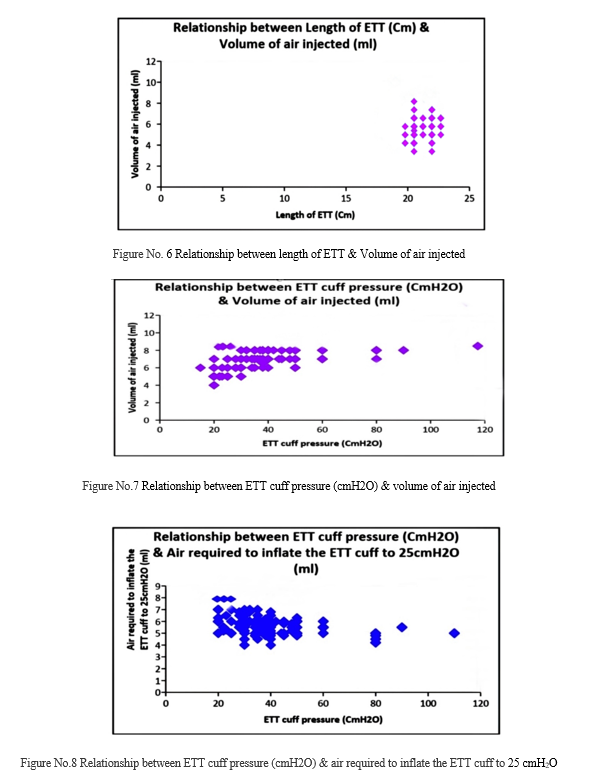
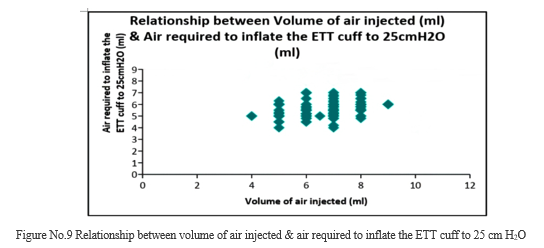
The Pearson correlation coefficient was employed to evaluate the relationships among several variables related to endotracheal tubes (ETT): ETT size, ETT length, ETT cuff pressure, and the volume of air injected into the cuff. The analysis revealed that the p-values for all relationships, except for the one between ETT size and cuff pressure, were < 0.05. This indicates that, generally, there are significant relationships among these variables, with the exception of ETT size and cuff pressure, which showed no significant correlation with the” r” value ( -0.015) and “p” value (0.103) i.e. > 0.05.
In more detail, the lack of a significant relationship between ETT size (measured by internal diameter) and cuff pressure suggests that the size of the ETT does not affect the pressure within the cuff. However, the relationships among the other variables—ETT size, ETT length, the volume of air injected, and the volume of air needed to inflate the cuff to 25 cmH2O—were statistically significant, indicating some level of association. Despite this, it is important to note that these associations, while positive and linear, were overall weak. This means that although there is a relationship, it is not particularly strong.
The data provided clear evidence of an association between the length of the ETT and the volume of air required to inflate the cuff to a pressure of 25 cmH2O. This suggests that longer ETTs may require more air to achieve the desired cuff pressure. Similarly, there was a close association between the volume of air injected into the cuff and the internal diameter (size) of the ETT. Larger internal diameters likely necessitate more air for proper inflation.
Furthermore, the study found that the average difference between the actual volume of air used to inflate the cuff to 25 cmH2O and the volume of air theoretically required was 1.03ml. This difference varied, ranging from 6.75 ml to 5.72 ml. This variability indicates that in some cases, significantly more or less air than expected was used. When broken down by gender, the average difference for male patients was 1.18 ml, while for female patients, it was slightly higher at 1.25ml. This gender-based difference suggests slight variations in cuff inflation requirements between male and female patients.
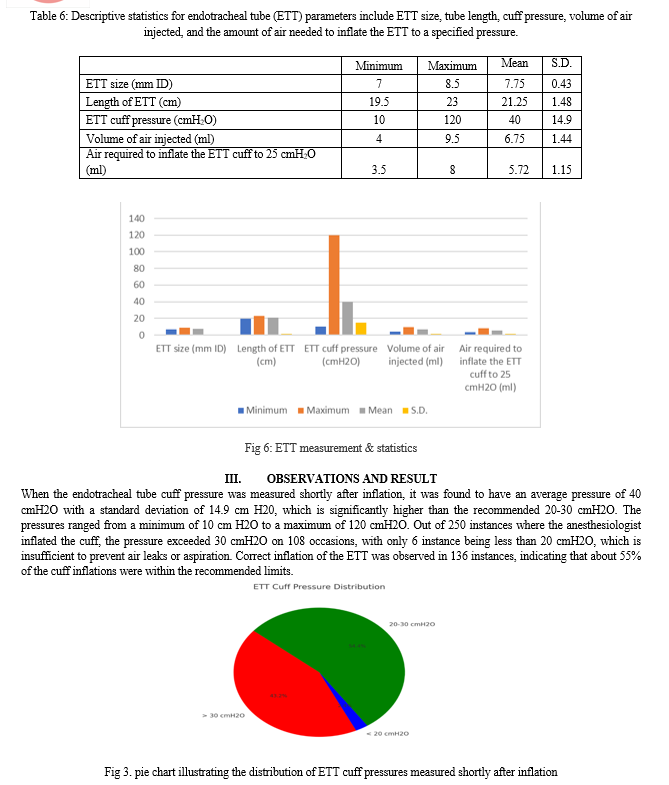
In our study Out of 250 instances where the anesthesiologist inflated the cuff, the pressure exceeded 30 cmH2O on 108 occasions, with only 6 instance being less than 20 cmH2O, which is insufficient to prevent air leaks or aspiration. Correct inflation of the ETT was observed in 136 instances, indicating that about 55% of the cuff inflations were within the recommended limits.
V. DISCUSSION
In our study 250 adult patients scheduled for elective surgery under general endotracheal anaesthesia to find the optimal air volume needed for inflating the cuff of an endotracheal tube cuff to 25 cmH2O, the amount of air injected by the practicing anaesthesiologist, and the discrepancy between the air volume required to achieve the prescribed cuff pressure.
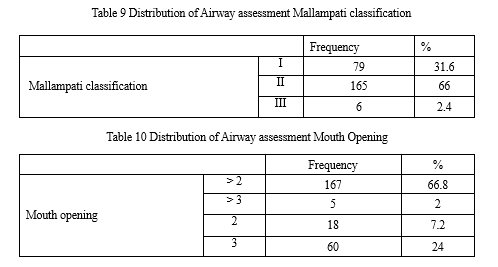
All 250 patients who participated in the study followed the protocol to complete and were included in the analysis. The results showed us that the average age of the study population was 43.34 years. In comparison the average age of the Indian population is around 30 years. This indicates a variation between the average age of the general population and those who attended the hospital, suggesting that the study sample may not accurately represent the general population. However, since our focus is solely on the hospitalized population, this difference may not significantly impact our analysis. Therefore, we need to specifically examine the average age of the population admitted to the hospital, particularly for surgical interventions.
Our analysis let out that the average weight of the study population was 56.50 kg, with males averaging 63.15 kg and females 57.83 kg. In against the average weight of Indian urban males is approximately 60 kg and females around 55 kg. Therefore, the weights observed in our study are slightly higher than the general population. It's important to note that demographic factors can vary based on region, the specific population served, and the types of surgical procedures involved. This difference might be more significant when comparing to a rural population. However, if both urban and rural populations are considered, the disparity may be reduced.
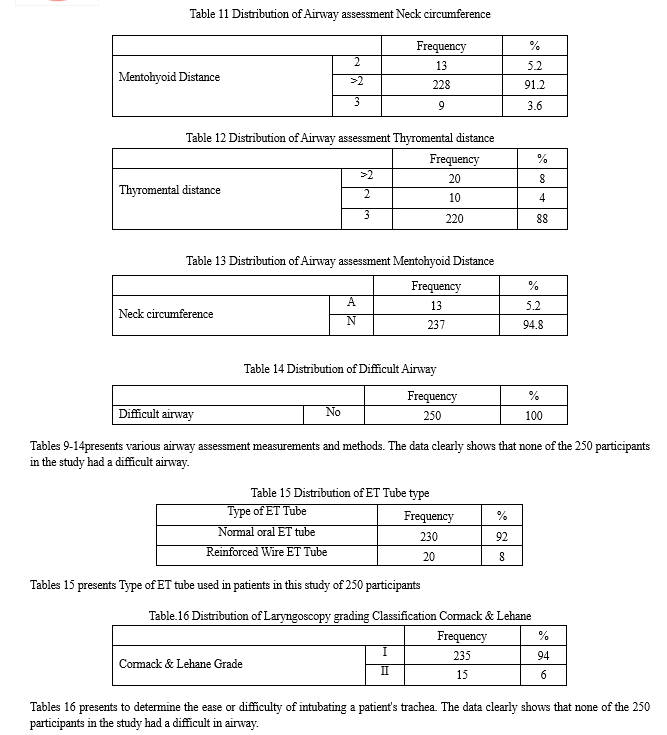
Likewise, the average height of our study population exceeds the national average for both males and females in India. The male participants had an average height of 169.49 cm compared to the Indian average of 165 cm, while the female participants averaged 163.77cm in height compared to the national average of 159cm. The combination of height and weight is a significant factor in determining the ease of intubation, making it essential to have a sample comparable to the general population to generalize the results effectively.
The average body mass index (BMI) of the male participants was 24.54kg/m², while the female participants had a BMI of 24.95 kg/m². In contrast, the average BMI for the urban Indian population is 22.2 kg/m² for men and 23 kg/m² for women, which is significantly lower than the BMI observed in our study population.
We selected endotracheal tubes (ETTs) with internal diameters of 8 mm or 8.5 mm for male patients, and 7 mm or 7.5 mm for female patients. On average, males received an 8 mm ETT, while females received a 7.5 mm ETT. This suggests that the majority of male patients were able to use the standard ETT sizes, but a significant number of female patients required smaller ETTs. The size of the ETT is important because it influences the volume of air needed to inflate the cuff and ensure a proper seal between the ETT and the tracheal wall.
Traditionally, the endotracheal tube (ETT) is secured at the angle of the mouth based on a predetermined length or after confirming bilateral air entry. Commonly, the ETT is fixed at approximately 21.6 cm in males and 21 cm in females. Although these standards were developed for a Caucasian population, our findings validate these practices. When the ETT is correctly positioned in the mid-trachea, the length from the tip to the angle of the mouth is 22 cm in men and 21.1 cm in women. The difference between these prescribed and measured lengths suggests variations in tracheal or neck length between different racial groups.
It was noteworthy that, in nearly all instances, the ETT cuff was overinflated, even by experienced anaesthesiologists. The average ETT cuff pressure was consistently higher than intended for both male and female patients. However, the average intracuff pressure was greater in female patients compared to males. This discrepancy can be attributed to two main factors: the relationship between the ETT cuff and the tracheal inner diameter, which is generally wider in males. The inner diameter of the trachea in males ranges from 15 to 25/ mm, whereas in females it ranges from 12 to 21 mm. This relationship is often not considered when selecting the ETT size for different sexes. Consequently, the space between the outer surface of the ETT and the inner surface of the trachea is smaller in women, requiring a lesser volume of air for similar inflation. This finding was confirmed in the current study, where the average volume of air needed to inflate the tracheal cuff to 25 cmH2O was lower in female patients compared to males (37cmH2O vs. 40 cmH2O).
L. Gilliland et al. 2 measured the endotracheal tube (ETT) cuff pressure of 96 adult patients undergoing general anaesthesia without nitrous oxide at CMJAH and CHBAH. Their study showed the mean ETT cuff pressure was 47.5 cm H?O, with a range of 10–120 cm H?O. In 64.58% of patients, ETT cuff pressures exceeded 30 cm H?O, while only 18.75% had pressures within the recommended range of 20–30 cm H?O. This was slightly similar to the findings of the current study.
Sengupta et al.3 found that ETT cuff pressure was on an average 35.3 ± 21.6 cm H2O, one hour into surgery, without using nitrous oxide. This was similar to the findings of the current study.2
Hoffman et al.4 In this study he found a near-perfect linear relationship between ETT cuff volume and pressure, with a correlation coefficient (r) of 0.969. This indicates that as the volume increases, the pressure also increases linearly without abrupt changes?.
"In our study, we found a strong correlation coefficient of 0.774 (p < 0.001), indicating a clear linear relationship between the volume of air injected and intracuff pressure. 5This underscores the importance of accurately controlling intracuff pressure. Despite inflation by experienced anaesthesiologists, ETT cuffs were frequently over-inflated. Previous research has shown that without pressure measurement devices, cuffs are often either incorrectly inflated or below recommended levels, posing risks such as laryngopharyngeal complications, gas leakage, inadequate ventilation, and potential aspiration." Following a comprehensive meta-analysis of nine studies involving 1077 participants, Hockey et al. concluded that an objective method of measuring intracuff pressure is essential to prevent cuff overinflation.6 This finding aligns closely with the results of the current study, which also underscores the necessity of precise intracuff pressure monitoring to ensure patient safety and optimize clinical outcomes. Furthermore, the adoption of standardized measurement techniques can enhance the consistency of care and potentially reduce the incidence of complications associated with cuff overinflation.
Maboudi et al. highlighted the significant impact of operator training on achieving optimal cuff inflation levels7. Initially, their study observed that untrained nurses consistently inflated endotracheal tube cuffs to excessively high pressures (>35 cmH2O). However, after receiving proper training, these nurses were able to adjust the cuff pressures to much safer and more acceptable levels in most cases, demonstrating the value of education in improving clinical practices. Top of Form
In this study out of 250 instances where anaesthesiologist’s inflated cuffs, the pressure exceeded 30 cmH2O on 108 occasions, with only 6 instances where it was below 20 cmH2O. which is insufficient to prevent air leaks or aspiration. Correct inflation, within recommended limits, was achieved 136 instances representing 55% of the cases. Despite the technique's variability, the consultants demonstrated fairly good accuracy. Under-inflation and its complications are unlikely because anaesthesia workers tend to slightly overinflate the cuff to ensure proper lung ventilation and prevent aspiration. Given the serious consequences of complications, overinflation is generally more advantageous than underinflation. Hockey et al. with moderate evidence, concluded that measuring ETT cuff pressure objectively reduces postoperative laryngopharyngeal symptoms and complications. However, this aspect was not covered in the current study.6
Interestingly, there was a noticeable tendency to overinflate the ETT cuff more in female patients compared to their male counterparts, although this difference did not reach statistical significance, with pressures averaging 37 cm H2O for males and 40 cm H2O for females. The higher average inflation pressure observed in female patients can be plausibly explained by the smaller volume of the cuff used in their ETT, which is inherently smaller due to anatomical differences. As a result, a relatively greater volume of air was required to achieve inflation.
Moreover, the anatomical differences between the tracheas of men and women play a significant role in this observation. Men typically have larger tracheal dimensions compared to women. However, the relationship between the ETT size and the tracheal diameter is not as straightforward as one might assume.
This complexity is highlighted by the finding that the average volume of air required for optimal cuff inflation was slightly lower in female patients. Specifically, male patients needed an average of 6.05 ml of air, while female patients required 5.45 ml, a difference that is statistically significant (p< 0.001).
These findings suggest that the anatomical interplay between the ETT and the trachea differs between genders, affecting the volume of air needed for cuff inflation. Despite this, the specific nature of these anatomical interactions remains underexplored, pointing to an area ripe for future research. Further studies could delve into the detailed mechanisms behind this phenomenon, potentially leading to more tailored and effective approaches to ETT cuff inflation in male and female patient.
In the present study, there was a direct relationship between the internal diameter (ID) of the endotracheal tube (ETT) and the volume of air required to inflate the cuff, with a correlation coefficient (r) of 0.885.
Our study boasts several strengths. We compared the volume of air used by an experienced anaesthesiologist, who inflated the ETT cuff based on their judgment, with the volume of air required to achieve an intracuff pressure of 25 cm H2O, when measured objectively. This comparison provided valuable insights into the volume of air necessary to safely inflate the ETT cuff to the recommended pressure of 25 cm H2O. The selected pressure was informed by the findings of Seegobin and van Hasselt, who advocated for an inflation pressure between 20 and 30 cm H2O.8
In this study, we measured both the actual volume of air injected and the volume required to reach the preset pressure. These measurements will help consultants refine their techniques in the future.
However, the study revealed a direct proportionality between the volume of air injected and the resulting intracuff pressure. This finding is crucial for refining clinical practices to ensure optimal intracuff pressure. Notably, the analysis distinguished between male and female patients, a significant factor given the anatomical differences in tracheal dimensions and the sizes of ETTs used for each sex. By doing so, the study addresses a gap in previous research, where investigators did not separate data by sex, thereby reducing the applicability and generalizability of their findings. This nuanced approach enhances our understanding and offers more tailored insights into ETT cuff inflation practices.
Some limitations of the study include not monitoring intracuff pressure intraoperatively to observe trends and changes, which are known to fluctuate during anesthesia. Additionally, recording postoperative symptoms and correlating them with intracuff pressure would have improved the clinical relevance of the results.
Although the number of participants was sufficient to power the study, including more participants could have made the findings more generalizable. Furthermore, excluding participants who required different sized ETTs or analysing participants based on the most appropriate ETT size would have allowed for determining the exact volume of air needed to inflate the cuff to the prescribed pressure, which could then be applied in daily practice
Conclusion
There was a common problem of overinflating the ETT cuff, resulting in high intracuff pressure. The recommended volume of air for optimal inflation of the ETT cuff was approximately 6.05ml for men and 5.45 ml for women. The cuffs were found to be overinflated in 43% of cases. This underscores the need to implement objective monitoring of ETT cuff pressure as a standard practice in clinical settings, thereby enhancing patient safety and reducing the incidence of associated complications. Incorporating these practices into routine care protocols can significantly improve patient outcomes and contribute to the overall quality of anaesthesia management in clinical settings.
References
[1] Timmermann A, Russo SG, Eich C, Roessler M, Braun U, Rosenblatt WH, et al. The out-of-hospital esophageal and endobronchial intubations performed by emergency physicians. Anesth Analg. 2007;104:619–23 [2] Endotracheal tube cuff pressures in adult patients undergoing general anaesthesia in two Johannesburg academic hospitals L Gilliland,H Perrie &J Scribante [3] Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol 2004; 4:8. [4] Linear Correlation of Endotracheal Tube Cuff Pressure and Volume Robert J. Hoffman, MD, MS,* Jefrey R. Dahlen, MD,* Daniela Lipovic, DO,* and Kai M. Stürmann, MD [5] ?ahiner Y. Indications for Endotracheal Intubation. Tracheal Intubation. 2018 Jul 25:59 [6] Does objective measurement of tracheal tube cuff pressures minimise adverse effects and maintain accurate cuff pressures? A systematic review and meta-analysis C. A. Hockey*, A. A. J. van Zundert†, J. D. Parat [7] Maboudi A, Abtahi H, Hosseini M, Tamadon A, Safavi E. Accuracy of endotracheal tube cuff pressure adjustment by fingertip palpation after training of intensive care unit nurses. Iranian Red Crescent Medical Journal. 2013 May;15(5):381. [8] Aspiration beyond endotracheal cuffs Ronald D. Seegobin & Gillian L. van Hasselt
Copyright
Copyright © 2024 Urfeena Gani, Basiet Ali. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

Download Paper
Paper Id : IJRASET63775
Publish Date : 2024-07-27
ISSN : 2321-9653
Publisher Name : IJRASET
DOI Link : Click Here
 Submit Paper Online
Submit Paper Online

